In this month’s blog we continue with Frank’s story. Frank is the senior from last month’s blog who, despite everyone’s best intentions, ended up stuck on a conveyor belt between the ER and home, and back to the ER again.
We want to help our readers understand any missed opportunities to improve Frank’s experience – and to illustrate the difference between health care and self-care. Improving healthcare in Canada is a very large, complex issue, but the biggest problem we are facing is the lack of clarity regarding the system’s boundaries. People assume too much and then, when we need to access the system the boundaries are made known to us. The reality is a shock.
Because Frank was in Ontario, we begin by looking at a general overview of what OHIP covers in certain circumstances.
Generally, as people age they need to be seen by a GP. Finding a GP is your responsibility. Visits with a GP are covered. Hospital visits, including nursing, diagnoses, blood test and x-rays, and some medications are covered. Any on-going personal care while in a hospital is not covered (continence management, personal hygiene, laundry, entertainment and snacks, etc.) Note that not all ambulance services are covered. For example, if your trip originates outside of Ontario, you are responsible for the full cost of the service.
OHIP covers “medical” needs, therefore it is safe to conclude that self-care that goes along with the reality of aging – fall prevention, nutrition, hygiene, continence management – are all private responsibilities.
HOME CARE – breaking down what OHIP provides
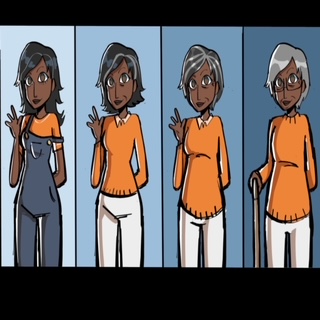
So far it is fairly straightforward, things get tricky when the Ontario Ministry of Long Term Care asserts that it “provides support for people in their homes”. Let’s break that down. What they really mean is you might qualify for a weekly 1 hour visit for assistance with showering, sometimes if someone is quite incapable of self-care, they may receive 3 – 1 hour visits. During those 1 hour visits, which includes travel, the caregiver will manage continence and try to do anything else that can be done within an hour. Keep in mind, the government’s resources are managed by HCCSS case workers, and that person assesses what is needed.
LONG TERM CARE – eligibility is determined by the government
If a senior is unable to compete 4/5 “activities of daily living” he or she will be considered eligible for Long Term Care (government subsidized care facilities). Activities of daily living include – personal hygiene, basic mobility (able to get in and out of bed, get around the house); going to the bathroom without assistance, able to dress independently, eat and drink without assistance. If eligible, families make 5 choices. Once a bed in one of the 5 selected residences is available the family has 24 hours to accept the bed. Unfortunately, since COVID, people in the community (not in the hospital) are rarely considered “in crisis” and therefore are not eligible for a bed in Long Term Care.
BILL C-7 – what this means for families
The government’s answer to “fixing” healthcare is naturally focused on providing medical services, which therefore gives priority to freeing up beds. If a senior no longer requires medical help, but help with “activities of daily living” instead, the senior can be forced to accept a bed in any LTC facility within a certain radius, regardless of the family’s preferences. If the senior or family refuses the move, they are charged up to $1800/day for a continued hospital stay.
The bottom line – know your responsibilities and make a plan for the “what if’s” of aging. What if I need care in my home? What if I can’t stay in my home? What if I can’t manage dressing myself anymore?
While ER visits (with the hope of admission) provide some respite, it is not a long-term solution. The “care beyond the scope” then usually falls to family members to figure out. For Frank this meant his elderly wife became the caregiver, and his family was left assessing his health to determine next steps – difficult without a healthcare degree, but absolutely necessary for advocating. In Frank’s case there was also a need for assistance with toileting – which for Frank’s family was too physically demanding. This, unfortunately, is not something the government will assist with – ever. It is a sad truth. A private caregiver was necessary in this case to alleviate the demands on Frank’s wife. While ideally we wish for kind, dignified nursing care in our golden years, that is something we must plan and pay for ourselves.
For Frank, his family, believed, as many of us do, that the system would provide more guidance and more care. In the next blog we can speak about how to plan for the days when people need non-medical care.